Abstract
Introduction: The tumor microenvironment (TME) has a significant impact on the development and evolution of multiple myeloma (MM). Understanding the reciprocal interactions between aberrant clonal plasma cells and the TME is required to shed light on the mechanisms behind disease progression from early (monoclonal gammopathy of undetermined significance (MGUS)/smoldering MM (SMM)) to active disease. γδ T cells are among the bone marrow infiltrating cells that have both innate and adaptive immune cell features and play a significant role in cancer immunosurveillance. To date, however, their contribution to the evolution of MM remains unknown. To this aim, we investigated the role of γδ T cells in MM and its early stages, developing the first single-cell (sc) atlas of this population in this disease.
Methods: CD3+ cells from the bone marrow of healthy donors (HD; n=3), MGUS/SMM patients (n=5), and active MM patients (n=9) were sorted and seeded into single drops using a Chromium instrument (10X genomics), and 12527 γδ T cells were analyzed using scRNAseq. To validate transcriptomic findings, we next isolated peripheral blood mononuclear cells (PBMCs) and bone marrow mononuclear cells (BMMCs) from healthy donors (n=4; PBMCs exclusively), MGUS/SMM (n=8), and MM patients (n=14) by density gradient centrifugation and performed flow cytometric analysis to evaluate the frequency, differentiation/exhaustion profile, and functionality of the two main γδ T cell subsets known as Vδ1+ and Vδ2+ T cells.
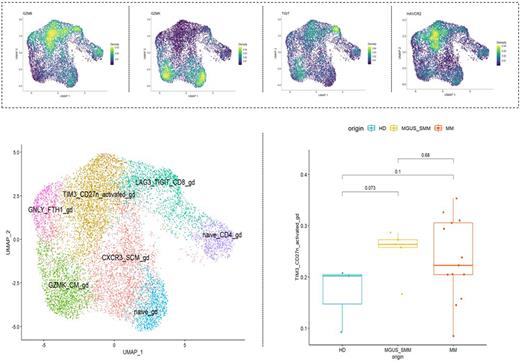
Results: Bioinformatics workflow enabled us to identify 7 γδ T clusters: 2 naïve subpopulations (CD4-/CD8- and CD4+ γδ T cells), 2 GZMB effector/terminally differentiated subpopulations (CD8+/TIGIT+/LAG3+, TIM3+/CD27- and GNLY+/FTH1+ γδ T cells) and 2 GZMK memory subpopulations (GZMK+ and CXCR3+ γδ T cells). Surprisingly, we observed a decrease in naive γδ T cells (p<0.05), which was coupled with an increase in TIM3 expression as MM evolved (Figure 1). Notably, we found a decrease in Vδ2+ T cells compared to healthy donors (mean 2,3% HD vs 1% MGUS/SMM vs 1,3% MM; p<0.05), as well as an increase in the Vδ1+/Vδ2+ ratio throughout MM progression (mean 0,4 HD vs 4,4 MGUS/SMM vs 4,4 MM). The frequency of Vδ2+ T cells in MM patients was positively correlated with free kappa light chain serum levels (PB: r= 0.8303, p<0.01; BM: r= 0.7455, p<0.05), instead, Vδ1+/Vδ2+ ratio was inversely correlated (PB: r= -0.7455, p<0.05; BM: r= -0.8909, p<0.01). Furthermore, we confirmed by flow cytometry the predominance of effector memory (Vδ1+ T cells: mean 1,4% HD vs 2.2% MGUS/SMM vs 14,4% MM; Vδ2+ T cells: mean 22,1% HD vs 21,4% MGUS/SMM vs 41,7% MM; p<0.05) and terminally differentiated γδ T cells (Vδ1+ T cells: mean 28,2% HD vs 79,2% MGUS/SMM 72,8% MM; Vδ2+ T cells: mean 19,2% HD vs 42,8% MGUS/SMM vs 32,2% MM; p<0.05) in MM patients as compared to healthy donors, where naïve (Vδ1+ T cells: mean 53,7% HD vs 15% MGUS/SMM vs 5,8% MM; Vδ2+ T cells: mean 10,5% HD vs 14,1% MGUS/SMM vs 8,1% MM; p<0.05) and central memory populations predominated (Vδ1+ T cells: mean 16,5% HD vs 3.4% MGUS/SMM vs 6,8% MM; Vδ2+ T cells: mean 48,7% HD vs 42,8% MGUS/SMM vs 17,2% MM; p<0.05). Accordingly, the analysis of exhaustion markers corroborated the progressive increase of TIM3 expression (but not PD1) in both Vδ1+ (mean 5,65% HD vs 34,5% MGUS/SMM vs 36,4% MM; p<0.05) and Vδ2+ T cell subsets (mean 2,1% HD vs 22,8% MGUS/SMM vs 32,6% MM; p<0.05). Finally, we observed that the acquisition of this exhausted phenotype along MM evolution was associated with impaired functions of both Vδ1+ and Vδ2+ T cells with reduced TNF-α (mean 75,1% HD vs 14,4% MGUS/SMM vs 14,5% MM; p<0.01) and IFN-γ (mean 28,8% HD vs 7,02% MGUS/SMM vs 7,24% MM; p<0.05) expression after in vitro stimulation.
Conclusions: These findings suggested that the upregulation of the immunosuppressive receptor TIM3 may play a role in destabilizing γδ T cells and inducing their dysfunction throughout the progression of MM. Furthermore, because PB-derived T cells mirrored the bone marrow landscape, monitoring them could provide a potential minimally invasive approach for identifying patients at high risk of progressing to symptomatic MM.
Disclosures
Paiva:Gilead: Honoraria; Sanofi: Consultancy, Honoraria, Research Funding; GSK: Honoraria, Research Funding; EngMab: Research Funding; Janssen: Consultancy, Honoraria; Amgen: Honoraria; Adaptive: Honoraria; Roche: Honoraria, Research Funding; Takeda: Honoraria, Research Funding; Bristol-Myers Squibb-Celgene: Consultancy, Honoraria, Research Funding; Oncopeptides: Honoraria. Siragusa:Csl Behring, Takeda, Amgen, Novartis, Bayer, Sobi, Novo Nordisk: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal